OU Health Stephenson Cancer Center has announced a historic first for the campus and the state: A new cancer drug, called OK-1, which was conceived and created by an OU College of Medicine researcher and developed entirely in Oklahoma, without the support of a pharmaceutical company, is being tested in humans for the first time in a Phase 1 clinical trial.
The drug was created by researcher Doris Benbrook, Ph.D., whose work on the compound began more than 25 years ago. New drugs developed within an academic institution, without the aid of a pharmaceutical company, are exceedingly rare. The Food and Drug Administration approved the drug to be given to humans in the clinical trial, which is underway at Stephenson Cancer Center. The drug is initially being given to women with advanced-stage ovarian, endometrial and cervical cancer.
“It is very exciting to reach the point where we can test OK-1 in a clinical trial,” said Benbrook, who is a professor in the Department of Obstetrics and Gynecology in the OU College of Medicine. “This drug is not available anywhere else in the world right now. We believe it has tremendous potential for treating cancer without causing toxic side effects.”
OK-1 is derived from the natural compound vitamin A. The human body uses vitamin A to make retinoic acid, a nutrient that supports healthy functioning. Some forms of retinoic acid, as well as synthetic versions called retinoids, have been used to treat cancers such as leukemia. However, both are highly toxic, Benbrook said, and patients often become resistant to their effectiveness. Her aim was to create a better version of the drug that is able to kill cancer cells but is less toxic to normal cells.
That effort has taken over two decades of experimentation. Benbrook worked with a collaborator to modify the drug’s chemical structure and test the biological activity of new versions. The new drug they ultimately developed has been modified to such an extent that it works in a completely different way than vitamin A. Collaborators in the OU College of Pharmacy performed research that was necessary to test OK-1 in clinical trials. The work has been supported by millions of dollars in grants from the National Cancer Institute.
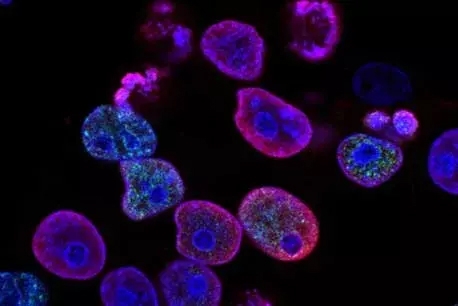
OK-1 works by taking away one of the “tricks” that cancer cells use to survive. When cancer cells develop, the body naturally tries to stop their invasion and growth. In response, cancer cells increase their production of “chaperone proteins,” which act like “bodyguards” to keep the cancer cells from dying. The drug OK-1 is able to attach to the chaperone proteins, disabling them in the process. The body’s immune system, or another drug like chemotherapy, is then better able to kill cancer cells because they are no longer protected by “bodyguards.” The drug does not harm healthy cells because they do not need the chaperone protection.
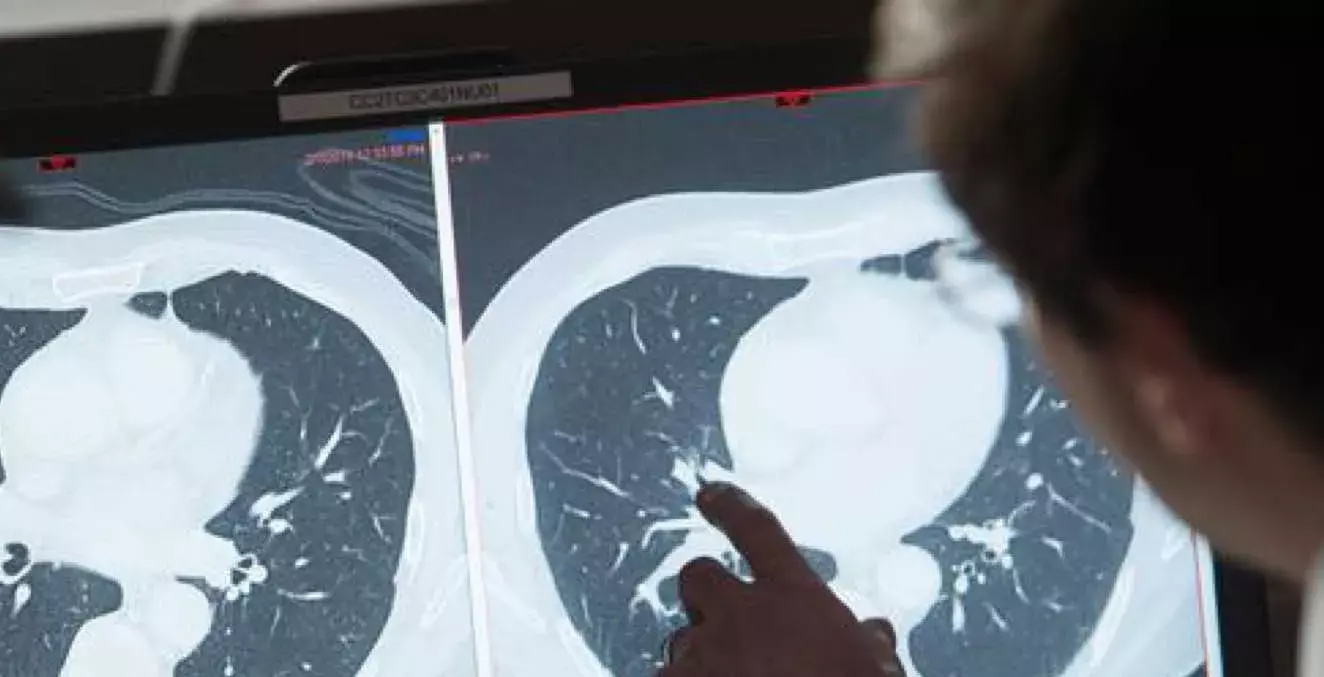
Phase 1 clinical trials are conducted to determine the highest dose of a new drug that can be given safely without causing severe side effects. While OK-1 has been tested extensively in the laboratory and in animal research models, the true effect can’t be known until it is given to humans. However, preclinical studies of the drug have proved that it is effective without causing severe side effects or birth defects, Benbrook said. The drug is being given to humans in capsule form.
Kathleen Moore, M.D., Associate Director of Clinical Research and Director of the Oklahoma TSET Phase 1 Program at Stephenson Cancer Center, is leading the clinical trial. “The Phase 1 investigators are so excited to finally have this novel drug available to our patients,” Moore said. “It is a completely new class of drug, which, in addition to having efficacy in and of itself, may help other current cancer therapies work better without adding toxicity. This is kind of the holy grail. We have many combinations that work better than the single drug, but the combinations are far too toxic for general population use. OK-1 gives us the opportunity to bring combinations into trials that may work better without compromising safety. The potential is so exciting.”
At the conclusion of the Phase 1 trial, Moore and her team will have learned the optimal dose of OK-1. In subsequent trials, they plan to test the drug in combination with other cancer drugs already on the market. Benbrook has made patent applications on several drug combinations; OK-1 appears to be most effective when given with other existing drugs.
“We found in our experimental models that when we add OK-1 to other cancer therapies like paclitaxel, which is the standard chemotherapy for endometrial cancer, we get a synergistic effect that is much better than either drug alone,” Benbrook said.
Benbrook’s preclinical research also has shown that OK-1 may be effective for preventing cancer. She plans to test OK-1 in an ovarian cancer prevention trial in the Cancer Prevention Clinical Trials Network, a program of the National Cancer Institute. The drug will be given to women who are going to have their fallopian tubes surgically removed. Because most ovarian cancers originate in the fallopian tubes, researchers will examine the effect of the drug on fallopian tube tissues. Ultimately, the drug could be given to women who are genetically predisposed to cancer, such as those with a BRCA gene mutation.
The Oklahoma TSET Phase 1 Program at Stephenson Cancer Center is the only such program in the state and is considered among the top 10 programs in the nation. As a National Cancer Institute-designated cancer center, Stephenson can offer patients first access to early-stage drugs like Benbrook’s OK-1.
“This is a very exciting time to be conducting the first Phase 1 trial for a drug developed on our campus,” said Robert Mannel, M.D., director of Stephenson Cancer Center. “It is only possible because of Dr. Benbrook’s passion and determination and the ability of Stephenson Cancer Center to offer Phase 1 clinical trials. We have a very special team of doctors, nurses, researchers and staff who work together to safely give these new drugs to humans.”
In addition to funding from the National Cancer Institute, Benbrook’s research has been supported by grants from Oklahoma City-based Presbyterian Health Foundation, as well as the OU College of Medicine Alumni Association.
This article was originally published by OU Health.