TULSA, OKLA. – Recently published research from the University of Oklahoma and the University of Tulsa shows that a new therapy for children with chronic nightmares reduced the number of nightmares and the distress they caused and increased the number of nights a child slept without waking. The study, published in Frontiers in Sleep, is thought to be the first randomized clinical trial to test a nightmare therapy in children, and it marks a step toward treating nightmares as a distinct disorder and not solely a symptom of another mental health issue.
Research suggests that one in six children with mental health difficulties suffers from chronic nightmares, an estimate that may be conservative because nightmares are rarely included in routine clinical screening. However, nightmares don’t always lessen when a child’s mental health disorder is treated. For example, nightmares are known to be a symptom of PTSD, but when children are successfully treated for their trauma, the nightmares don’t always diminish. That spurred the study’s authors to create and test a therapy to specifically address nightmares regardless of a child’s comorbidities.
“There is a lack of research on nightmares in children; most studies have been done in adults. We really want to get to the root of the issue because when kids suffer from nightmares, they’re scared to go to sleep, which makes them tired and irritable during the day, and they’re prone to behavioral problems – all of which can affect their functioning at school and in other areas of their lives,” said child and adolescent psychiatrist Tara Buck, M.D., an associate professor at the OU School of Community Medicine in Tulsa.
Buck directed the study with Lisa Cromer, Ph.D., a professor of psychology at the University of Tulsa and a volunteer child psychiatry faculty member at OU School of Community Medicine in Tulsa. Cromer led the development of the therapy, beginning with a pediatric adaptation of an adult nightmare therapy and refining it through pilot studies. The therapy comprises five weekly sessions that educate youth about the importance of sleep, create the motivation for habits that can improve sleep, and guide children to “rewrite” their nightmares into pleasant dreams.
Before treatment began, student participants received a box in the mail with items they would use during the study, including “boggle goggles” that help children better understand the effects of being sleep-deprived (the goggles’ traditional use is to demonstrate impairment from alcohol). Children also received a pillowcase and markers to write or draw pictures of things they wanted to think about at bedtime. Cromer and her team designed the treatment to be developmentally appropriate and interactive.
“The treatment uses cognitive behavioral therapy but also incorporates relaxation strategies, mindfulness, stress management and visualization to change the structure of dreams. We also help them create a plan to use if they do have nightmares so they can ‘change the channel’ and go back to sleep,” Cromer said. “At the core of the model is self-efficacy. Every unit teaches them that they can be the director of their dreams. We hypothesize that is the effective mechanism of change.”
The trial enrolled 46 youth from across Oklahoma ranging in age from 6 to 17, with an average age of 12. Notably, they had been having persistent nightmares for no less than six months and, in some cases, for years. Participants were randomly assigned to receive the treatment or to be in a control group that tracked their nightmares but received no therapy. Once the trial was complete, children in the control group were provided the therapy.
In addition to seeing a statistically significant reduction in nightmares, the research team also measured suicidal thinking related to nightmares. Previous research has shown a correlation between nightmares and suicidality in youth over time. In this study, five children in each group reported suicidal thinking at the start of the trial. At its completion, only one youth in the treatment group reported continued suicidal thoughts, compared to four in the control group.
Because the trial began during the COVID-19 pandemic, the study team modified the treatment for telehealth. The trial was designed with minimal exclusion criteria because Buck and Cromer wanted to test the therapy in a range of children, such as those who had ADHD or learning disabilities. Children with sleep apnea were excluded because their sleep problems needed medical attention.
In the future, Buck and Cromer would like to obtain funding to test their nightmare therapy in a larger trial that follows children over a longer period of time. They are also adapting the therapy for various ethnicities and cultures, and they’ve launched a study to screen for nightmares in a primary care setting. Their efforts represent a paradigm shift in pediatric care. In their training, neither was taught to ask about nightmares during a clinical visit, nor do children and families bring up nightmares.
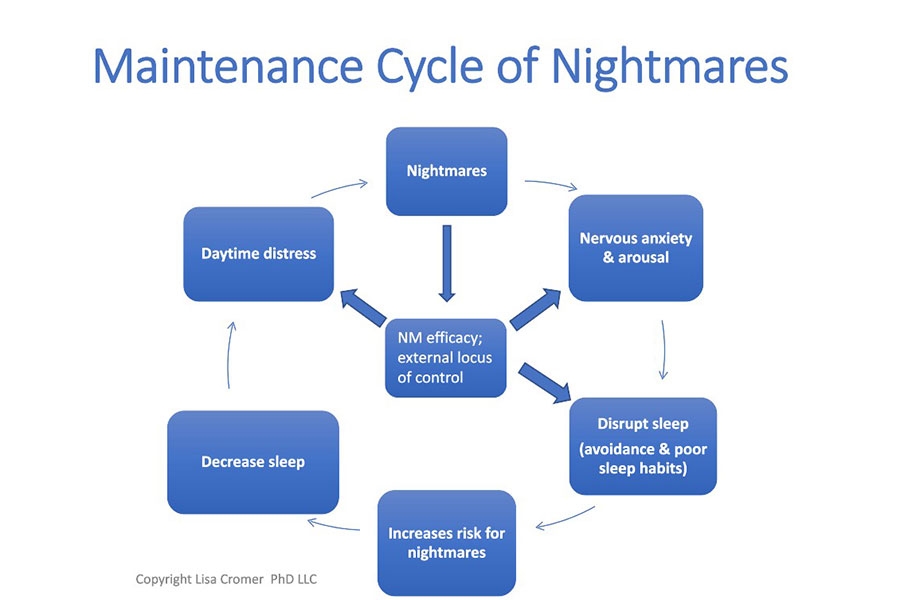
“We may talk about strategies for addressing a child’s anxiety during a clinical exam, but only now are we starting to address nightmares directly,” Cromer said. “Nightmares can trap children in a cycle. They remember the nightmare and may stay hypervigilant or avoidant at bedtime. Then, they don’t get enough sleep and become more anxious, which makes them more likely to continue having nightmares. It’s exciting to have a therapy that appears to significantly reduce nightmares and related distress.”
About the Project
The study can be found at https://www.frontiersin.org/journals/sleep/articles/10.3389/frsle.2024.1401023/full. Funding for the study was provided by the Oklahoma Center for Advancement of Science and Technology, the OU College of Medicine Alumni Association, and the University of Tulsa Office of Research and Sponsored Programs Faculty Research Grant.
About the University of Oklahoma
Founded in 1890, the University of Oklahoma is a public research university with campuses in Norman, Oklahoma City and Tulsa. As the state’s flagship university, OU serves the educational, cultural, economic and health care needs of the state, region and nation. In Oklahoma City, OU Health Sciences is one of the nation’s few academic health centers with seven health profession colleges located on the same campus. OU Health Sciences serves approximately 4,000 students in more than 70 undergraduate and graduate degree programs spanning Oklahoma City and Tulsa and is the leading research institution in Oklahoma. For more information about OU Health Sciences, visit www.ouhsc.edu.
To combat power outages and extreme weather events, a team led by University of Oklahoma researchers has helped launch a project utilizing electric school buses as a backup energy resource.
The University of Oklahoma Health Campus was recently recognized for its increased momentum in advancing discoveries that change lives, achieving the state’s first Top 100 national ranking based on funding from the National Institutes of Health, according to the Blue Ridge Institute for Medical Research. The ranking—the highest in OU’s history and in the state—solidifies the University’s position as the state’s leading driver of health-related research.
Stefano Tarantini, an assistant professor in the Department of Neurosurgery at the University of Oklahoma College of Medicine, spends his days in the laboratory searching for answers to the cognitive decline that too often plagues older adults.