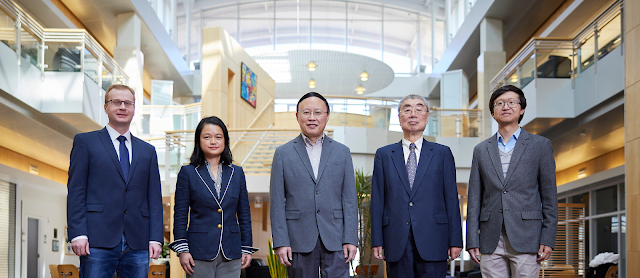
Left to right: Stefan Wilhelm, Han Yuan, Bin Zheng, Hong Liu, Yuchen Qiu
The University of Oklahoma has received funding from the National Institutes of Health to establish the Oklahoma Center of Medical Imaging for Translational Cancer Research, a collaboration between the Gallogly College of Engineering on the OU Norman campus and OU Health Stephenson Cancer Center in Oklahoma City.
“Great scientific advancements are best achieved through multidisciplinary collaboration, which is exactly what will be accomplished at the Oklahoma Center of Medical Imaging for Translational Cancer Research,” said OU President Joseph Harroz Jr. “This exciting effort unites some of the brightest minds from across two of our campuses, who will combine their expertise to develop life-changing solutions. Their work is a prime example of how OU researchers are reaching beyond traditional boundaries to spark new discoveries with real-world impacts.”
The award from the Centers of Biomedical Research Excellence (COBRE) program of the NIH is expected to provide more than $11.3 million over a five-year Phase 1 period, with the opportunity to compete for renewal for up to three phases. The first phase supports the center’s establishment to galvanize multidisciplinary biomedical research through equipment and facilities support to junior faculty. This is the second COBRE center on OU’s Norman campus, joining the Oklahoma COBRE in Structural Biology.
Bin Zheng, Ph.D., a professor and Oklahoma TSET Cancer Research Scholar in the Gallogly College of Engineering’s School of Electrical and Computer Engineering, is leading the new center.
About the Oklahoma Center of Medical Imaging for Translational Cancer Research
Medical imaging is an essential tool to help doctors and scientists assess the size and scope of a tumor that will be effectively removed by surgery, as well as the rate at which tumors shrink in response to medical interventions such as chemotherapy or radiation therapy. OU researchers are investigating multiple avenues to help improve medical imaging use in cancer detection, diagnosis and treatment.
“Radiological imaging tries to detect a tumor or disease area, while pathologic imaging tries to confirm whether it is benign or malignant,” Zheng said. “While there are other kinds of testing methods, like blood testing, imaging is the most commonly used by clinicians.”
“The problem is that reading medical images by radiologists is quite difficult because tumors, cancer and most diseases are very heterogenous – there is a lot a variation,” he added. “We often see different image diagnostic results from different clinicians or different hospitals because of the large inter-reader variability. This can result in applying different treatment options and potentially reduce treatment efficacy.”
To counter this challenge, the center’s researchers are developing quantitative imaging markers to provide an objective measure or index that can reduce subjectivity and improve consistency for medical image diagnosis using two primary types of research approaches.
The first approach is to develop new investigative cutting-edge imaging modalities to expand the ability of doctors to see or detect more detailed tumor internal structures such as using advanced optical imaging modalities and technology.
The second is to explore and extract more effective image features from the existing clinical imaging modalities – like CT, MRI and X-ray images – and then use artificial intelligence or machine learning models to develop new quantitative imaging markers to help reduce the subjectivity and variability of cancer diagnosis and predicting cancer prognosis.
“When some patients undergo cancer treatments, some will respond favorably while others do not. The tumor continues to grow, so if we can develop a quantitative imaging marker to predict a patient’s likelihood to respond to a certain kind of chemotherapy or treatment, we can help physicians explore an alternative approach that may be more effective,” Zheng said.
Current Projects
The center is beginning with four projects currently underway. Three projects are led by faculty in the Gallogly College of Engineering and one by a clinician scientist at the Stephenson Cancer Center. All four projects will include close collaboration between engineering researchers from the OU Norman campus and clinician scientists from the OU Health Sciences Center campus to promote interdisciplinary and translational cancer research.
Han Yuan, Ph.D., an associate professor in the Stephenson School of Biomedical Engineering at OU Norman, is leading the project, “Neuroimaging Markers for Predicting Outcome of Brain Surgery.”
Yuan will collaborate with two clinician-scientists, Chad Glenn, M.D., and Ian Dunn, M.D., in the Department of Neurosurgery at the OU College of Medicine. The researchers are using improved imaging modalities and quantitative markers to more clearly define the margin of a tumor to improve patient outcomes.
“Accurately determining the extent of tumor resection, the process of cutting out impacted tissue, has a significant impact on patients’ survival and risk of permanent post-operative neurological deficits,” Yuan said. “However, this is very difficult because tumors with ill-defined boundaries in proximity to critical brain areas are often incompletely removed or deemed inoperable for fear of damaging brain function.”
“We propose to develop a new approach to identify new quantitative image markers computed from three types of neuroimaging data using artificial intelligence, which enables us to more clearly define the margin of the tumor, predict the recovery of neurological deficits, and thus help improve surgical effect and survival of patients,” she said.
Stefan Wilhelm, Ph.D., assistant professor in the Stephenson School of Biomedical Engineering, is leading the project, “A New Ultrastructural 3D Optical Imaging of Tumor Endothelium for Cancer Nanomedicine Development.”
Wilhelm will collaborate with Stevenson Cancer Center breast cancer oncologist Wajeeha Razaq, M.D., and molecular biologist Resham Bhattacharya, M.D., at OU Health Sciences Center. The center will support the purchase of a 3D super-resolution optical microscope to allow researchers to better study nanomedicine, a branch of medicine that fuses nanotechnology and medicine for cancer treatment and prevention. The high-powered microscope will improve research in this area.
“Nanomedicine is a new and promising technology to improve drug delivery to tumors and treat cancer,” Wilhelm said. “However, the efficacy of nanomedicine still needs to be improved.”
“The objective of this project is to develop a 3D super-resolution optical microscope as a novel and unique method which enables researchers to better understand the intracellular pathways that nanoparticles take during transcytosis to treat tumors,” he added. “Success of this project can help researchers design and implement the optimal nanoparticle properties for intracellular nanoparticle transport and transcytosis to significantly improve the efficacy of drug delivery to tumor tissue in cancer treatment.”
Yuchen Qiu, Ph.D., an assistant professor in the School of Electrical and Computer Engineering, is leading the project, “Early-Stage Evaluation of Ovarian Cancer Prognosis Fusing Radiographic and Pathology Medical Imaging.”
Qiu will collaborate with an oncologist, Kathleen Moore, M.D., and a pathologist, Kar-Ming Fung, M.D., at OU Health. This project aims to use artificial intelligence and machine learning with current CT imaging and pathology data to develop a model that can inform the establishment of imaging markers that can reduce subjectivity and variability of imaging results and improve patient treatment.
“Chemotherapy is commonly used to treat ovarian cancer,” Qiu said. “However, ovarian cancer is highly heterogeneous, and tumor response to specific chemotherapy varies significantly among patients. Currently, it lacks accurate clinical markers to stratify patients and predict who can and cannot benefit from certain types of chemotherapy drugs.”
“In order to address and help solve this clinical challenge, we propose to develop and validate a new strategy for early prediction of tumor response to chemotherapy using a novel image marker generated by an artificial intelligence or machine learning model that is trained using image features computed from both radiographic CT images and digital histopathology images,” he added. “Our goal is to enable more accurate predictions of patients’ response to chemotherapy at an early stage, in four to six weeks after starting chemotherapy, which can significantly reduce unnecessary toxicity to those patients who do not respond to the specific chemotherapy and apply the alternative treatment.”
Lauren Dockery, M.D., a gynecologic oncologist and assistant professor in the Division of Gynecologic Oncology at OUHSC, is leading the project, “Using 3D Quantitative Optical Methods to Characterize Treatment of Ovarian Cancer.”
Dockery will collaborate with Qinggong Tang, Ph.D., an assistant professor in the Stephenson School of Biomedical Engineering. This project aims to use new investigative imaging methods, optical coherence tomography and full-field optical coherence tomography to test an exploratory cancer drug.
“Response rates of ovarian cancer patients to the traditional chemotherapy are often low in current clinical practice,” Dockery said. “To more effectively and efficiently address this clinical issue, repurposing drugs is an increasingly popular strategy in oncology due to the financial and logistical constraints of new drug development.”
Previous studies have shown that an anti-parasitic drug may have the potential to treat certain forms of cancer, including ovarian cancer, but more research is needed for scientists to better understand its effects.
“Despite initially promising results, the exact mechanism of its anti-cancer effect in tumor cells is unknown,” she said. “This project will provide important information regarding its anti-cancer effects and help determine the optimal mechanism of applying this promising anti-parasitic drug to more effectively treat ovarian cancer in a future clinical study.”
In each year of Phase 1 of the NIH COBRE program, the center will also support two new pilot research projects that can help junior faculty test theories and gain experience before going on to lead independent high-impact research.
Supporting Cores
Two supporting core research resources will also be established to build the necessary infrastructure to support current and future medical imaging-related research projects.
Medical Imaging Technology Development Core: Directed by Hong Liu, a Charles and Jean Smith Chair and professor in the School of Electrical and Computer Engineering, Gallogly College of Engineering. The objective of this core is to implement an interdisciplinary management plan to build the optimal infrastructure to support translational medical imaging-related cancer research. In addition to integrating the existing medical imaging equipment and resources from five electrical and computer engineering laboratories, the core will also involve new research and development tasks including designing and developing a series of investigative imaging tools and testbeds to provide researchers with fast and cost-effective methods to test concepts and hypotheses, and to build an integrated computer network and provide new computer-aided quantitative image feature analysis schemes and software to support researchers in conducting large data and deep transfer learning-based image informatics studies.
Research and service activities will be guided and supported by an advisory committee with broad expertise in the development and use of medical imaging technologies. Currently, the advisory committee includes three members from OUHSC: Salahuddin Ahmad, Ph.D., professor and director of medical physics residency in the Department of Radiation Oncology; Dee Wu, Ph.D., associate professor and the chief of technology applications and translational research in the Department of Radiological Sciences, and Theresa Thai, M.D., an assistant professor and assistant vice chair of clinical services in the Department of Radiological Sciences.
Clinical Imaging and Data Resource Core: Kathleen Moore, M.D., an associate professor of gynecology oncology and associate director for clinical research in the Stephenson Cancer Center of OUHSC, is the director. The objective of this core is to provide researchers with both regulatory and scientific support to facilitate their effort to conduct medical imaging-related translational cancer research projects. The core operation includes ensuring that researchers fully understand all NIH policies and regulations for the protection of human subjects and the welfare of vertebrate animals, certifying that study protocols for both retrospective and prospective studies are fully compliant with all NIH-mandated regulatory requirements, assisting with the IRB and IACUC protocol application writing and submission, providing biostatistics support to confirm that experiments are designed with appropriate statistical power and the proper statistical data analysis methods are used, and establishing a unique platform that can provide researchers with the shared databases allowing access to the linked annotated medical images, biospecimens and clinical data necessary to facilitate the progress of research projects.
The core also has an advisory committee with four members including Anthony Alleman, M.D., a Bob G. Eaton Chair in the Department of Radiological Sciences, Michael Talbert, M.D., a Lloyd E. Rader Professor and chairman of the Department of Pathology, Sara K. Vesely, Ph.D., a David Ross Boyd Professor of Biostatistics and an associate dean of academic affairs for biostatistics and epidemiology, and Joel Guthridge, Ph.D., a scientific director of the CAP-certified biorepository at the Oklahoma Medical Research Foundation.